Are your eyes red, gritty, painful, or irritated? If you’ve been struggling with these symptoms, you’re not alone. Millions of people worldwide suffer from dry eye syndrome, and many rely on eye drops without finding real relief. As someone who has spent time understanding and managing dry eyes, I want to share with you my insights and tips to help you find comfort and regain control of your eye health.
Understanding Dry Eyes
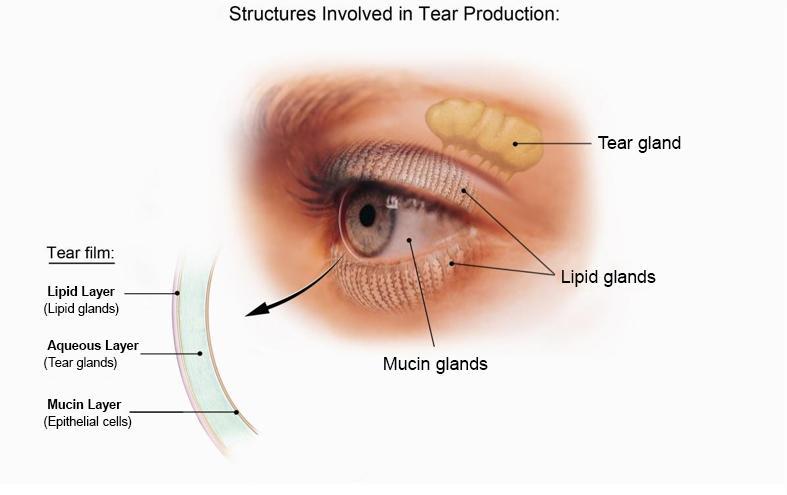
Dry eye symptoms occur when your eyes aren’t producing enough tears or the right quality of tears. Tears are crucial for keeping your eyes lubricated and protected. The tear film consists of three layers: mucus, water, and oil. These layers work together to keep the surface of your eyes moist. When this delicate balance is disrupted, it can lead to dryness, discomfort, and even vision problems.
When the tear film isn’t functioning properly, the surface of the eye can develop tiny pits or marks called punctate epithelial erosions. These erosions can cause irritation, pain, and even blurry vision. For many, artificial tears are the go-to solution, but they don’t always provide adequate relief—especially for those with severe dry eye.
Causes of Dry Eye
There are many reasons why someone might develop dry eye. It can be due to medications, autoimmune diseases, inflammation, or simply a natural decline in tear production as we age. In today’s digital world, screen time has become a significant contributor. When we stare at screens for long periods, we blink less frequently, reducing the natural spread of tears across our eyes. This can exacerbate dryness and discomfort, making it even more important to take steps to protect our eyes.
Strategies to Manage Dry Eye
I’ve found several strategies that work effectively to manage dry eyes, and I’ll share them with you below. These tips are practical and easy to incorporate into your daily routine.
Warm Compresses
Warm compresses are an excellent way to soothe dry eyes and improve the function of your meibomian glands, which are responsible for producing the oil layer of your tears. However, there’s a trick to doing it right. Don’t just use a regular towel, as it cools down quickly due to evaporation. Instead, you can place the warm towel in a Ziploc bag to retain the heat longer. Alternatively, you can purchase an eye mask with small beads that retain heat. These are available at stores like CVS, Walgreens, or even TJ Maxx. I found mine at TJ Maxx for just $5.

After heating the eye mask in the microwave, place it on your eyelids for about 10 minutes. This gentle heat will warm up your meibomian glands and help them secrete oil more effectively. For those with severe dry eye, I recommend using warm compresses three times a day. If your symptoms are mild, once a day or every other day might be sufficient.
Eyelid Hygiene
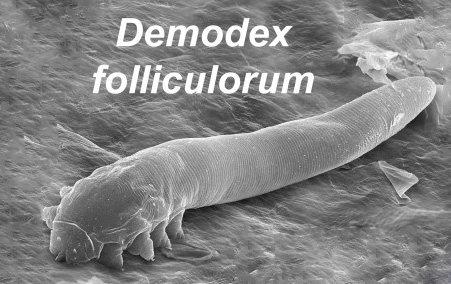
After using a warm compress, I like to clean my eyelids to remove any debris or buildup that might block the oil glands. A diluted solution of no-tears baby shampoo works perfectly for this. Simply mix the baby shampoo with water, dip a Q-tip into the solution, and gently clean along your lash line. Think of it as giving your eyelashes a gentle shampoo—something we often neglect. Regular eyelid hygiene can also help prevent issues like dandruff, debris buildup, or even parasites like Demodex that can clog the oil glands.
Artificial Tears
Artificial tears are another staple in managing dry eyes. There are many brands available, such as Refresh and GenTeal, and you may need to experiment to find the one that works best for you. If the artificial tears in bottles irritate your eyes, you might need to switch to preservative-free options that come in individual vials. These are particularly helpful for people with sensitive eyes and dry eyes associated with autoimmune diseases like Sjögren’s.
While artificial tears can provide temporary relief, it’s important not to rely solely on them. Combining them with other strategies, like warm compresses and eyelid hygiene, can significantly enhance their effectiveness.
Redness Relief Drops
Redness relief drops can be tempting when your eyes are looking bloodshot or tired, but they should be used sparingly. These drops work by constricting the blood vessels in your eyes, making them appear whiter. However, overusing these drops can lead to rebound redness, making your eyes look even worse when the effect wears off. I recommend saving redness relief drops for special occasions, like a business presentation or a social event. Better yet, ensure you’re getting enough sleep, as this can naturally reduce redness and improve your eye health.

When Home Remedies Aren’t Enough
Sometimes, home remedies and over-the-counter solutions aren’t enough to manage dry eyes, especially in severe cases. If you’ve tried warm compresses, eyelid scrubs, and artificial tears without success, it’s time to consider other options.
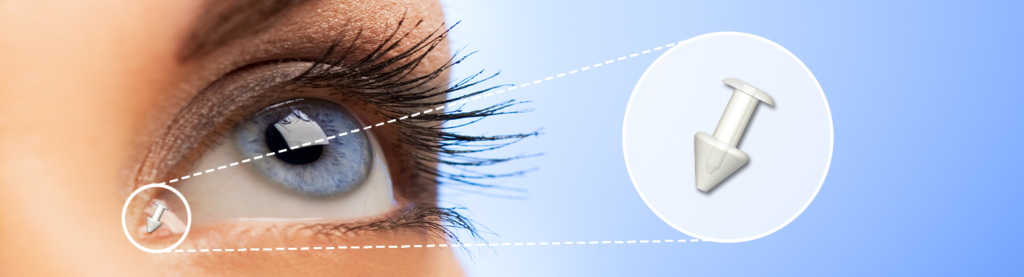
Punctal Plugs
Punctal plugs are tiny devices that your doctor can insert into your tear ducts to slow down the drainage of tears. By keeping your natural tears on the surface of your eyes longer, these plugs can provide significant relief. This is a simple and effective procedure that has helped many people with chronic dry eye.
Prescription Eye Drops
There are prescription medications, such as cyclosporine (Restasis), that can help reduce inflammation and improve tear production. While these medications can be expensive, they are often very effective. If you’re considering this option, check with your doctor to see if your insurance will cover it.
Intense Pulsed Light (IPL) Therapy
IPL therapy is a newer treatment option for dry eyes. It involves using intense light to stimulate the meibomian glands and improve oil production. While this treatment can be effective, it’s not always covered by insurance, and costs can range from several hundred to over a thousand dollars. Be sure to check with your insurance provider if you’re considering IPL therapy.

Autologous Serum Drops
For those with severe dry eye, autologous serum drops might be a game-changer. This treatment involves drawing your blood, spinning it down to separate the serum, and using that serum as eye drops. The nutrients and growth factors in the serum can help nourish and heal the surface of your eyes. This treatment is highly effective but may not be widely available, so consult your doctor to see if it’s an option for you.

Scleral Contact Lenses
Scleral contact lenses are a specialized type of contact lens often recommended for people with severe dry eye syndrome, as they create a fluid reservoir between the lens and the cornea. Scleral contact lenses effectively hydrate the eye and provide significant relief from dryness, irritation, and discomfort, essentially acting as a protective barrier over the corneal surface to prevent excessive tear evaporation.

Final Thoughts
Managing dry eyes requires a combination of strategies, and what works for one person may not work for another. Through trial and error, I’ve found that warm compresses, eyelid hygiene, and artificial tears form a strong foundation for dry eye management. For more severe cases, consulting a doctor and exploring advanced treatments like punctal plugs, cyclosporine eye drops, or autologous serum drops can make all the difference.
If you’ve found this guide helpful, I encourage you to take action and try some of these tips. Your eyes will thank you! And remember, if your symptoms persist, don’t hesitate to seek professional advice. Dry eye is a common condition, but with the right approach, relief is within reach. Thank you for reading, and I wish you comfort and clear vision ahead.


Leave a Reply